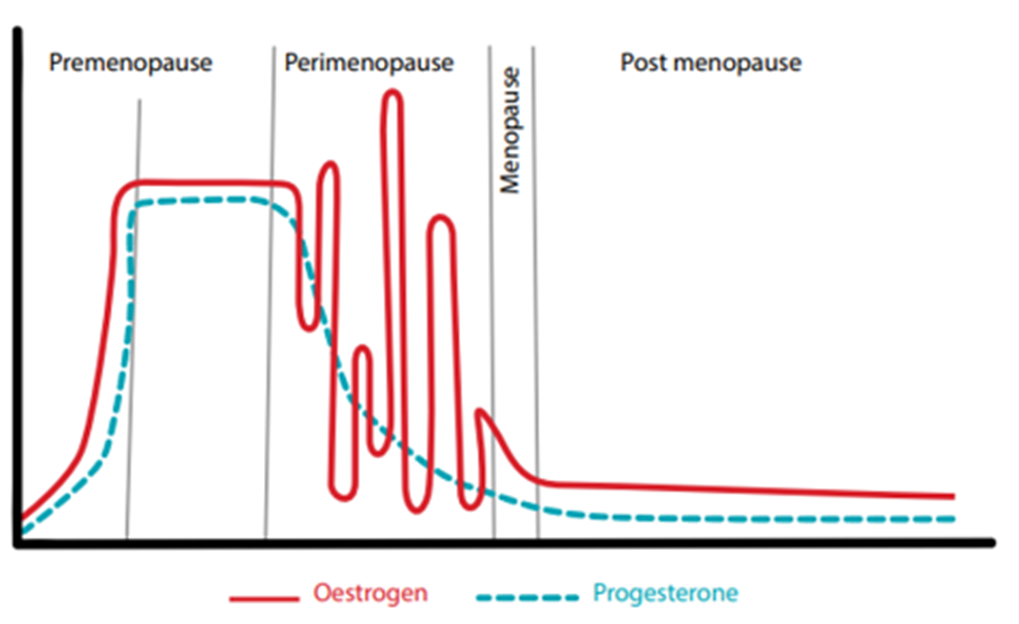
Menopause occurs when the female body makes fewer reproductive hormones and ultimately leads to periods stopping, although changes can occur in the years prior to this. This typically occurs between the age of 45 and 55.
The time before, when you start to feel the changes of menopause and changes to your period is called the perimenopause. Both can lead to physical and mental health changes, which may affect various aspects of your life.
Scroll down for more information or:

About menopause
The perimenopause and menopause are different for everyone. As hormone levels fluctuate during this time, it is normal to experience a number of changes and symptoms.
Determining changes in your period can be difficult, which can make it harder to diagnose perimenopause or menopause. This is especially true if you’re taking a regular contraceptive pill, have a coil, or have had certain surgeries, like an endometrial ablation.
Understanding what to expect and exploring ways to manage your symptoms can help you navigate the menopause transition with confidence.
Explore recommended reading to get you started on your menopause journey by Rock My:
A series of clinician-facing webinars have been held throughout 2024 and 2025 to support GPs to help women they see within their practice. All clinical staff are able to watch the recordings by accessing the secure area of the GP Alliance website.
Common menopause symptoms
Menopause changes not only feel different for everyone but as there are over 30 symptoms it is sometimes hard to work out whether your particular experiences are down to menopausal changes. They usually start months or even years before you reach full menopause and can change over time. This is normal, but getting early advice and support from your GP or nurse can help you to manage your health, relationships and work.
Some of the common changes you might expect to experience:
Contraception masking the menopause
You cannot know for sure whether you have reached menopause if you are using hormonal contraception like the pill, hormonal coil, contraceptive implant or contraceptive injection. This is because hormonal contraception can affect your periods. Visit the NHS website for more information about which contraception might mask symptoms of the menopause:
HRT
Your doctor may suggest prescription Hormone Replacement Therapy that can help with most menopause symptoms, such as hot flushes, mood swings and vaginal dryness. It can also help prevent weakening of the bones (osteoporosis).
Other prescribed medicines
Some other medications can help with difficult symptoms of the menopause like hot flushes and low mood. Talk to your doctor about other medicines that might be right for you.
Referral to specialists
Your doctor may suggest referring you to a specialist doctor or physiotherapist.
Alternatives to HRT
Complementary and non-medical therapies
Complementary and alternative treatments, such as herbal remedies are not recommended for symptoms of the menopause or perimenopause. Compounded bioidentical (“natural”) hormones should be avoided. This is because it is not known how safe they are. They can also interact or interfere with other medications.
Self-help
You can manage most menopause changes yourself – and there are plenty of resources available to help you:
Black and ethnic minority women
Your stories
LGBTQ+
How to live well
Perimenopause and menopause are excellent times to review your lifestyle. You may have been leading a healthy lifestyle up to this point but the change in hormones puts different strains on both your physical and mental health. To thrive throughout your menopause, try to maintain a balanced and healthy life including:
Reviewing your alcohol consumption, stopping smoking and managing stress are all things that can help to improve your experience of this time of life.
Eating a balanced diet
FAQs on weight gain, nutrition and lifestyle during the menopause
Menopause and sleep
Insomnia is a common experience during the menopause often with hot flushes and sweats.
Sleepio is the NICE-recommended online sleep improvement programme to help you clear your mind and get better sleep. It is clinically proven to help address the root causes of poor sleep and insomnia.
Getting active
Being more active can also help deal with menopause related symptoms.
Stopping smoking
A number of studies have taken place to understand the link between smoking and early menopause. It is generally agreed that smoking is more likely to bring forward the onset of menopause 18 months earlier for women who smoke compared to those who don’t.
Nicotine disrupts the conversion of a hormone within the body (androstenedione) to oestrogen which results in a dip in oestrogen levels, thus triggering early onset menopause. Smoking can also intensify menopausal symptoms.
Alcohol and menopause
Alcohol can increase some symptoms of perimenopause and menopause.
Menopause, sex, and relationships
Perimenopausal and menopausal symptoms can affect women in many different ways, and mental and physical symptoms can often be detrimental to relationships. But help is available.
For information on how your partner can best support you during menopause, refer them to The Menopause Charity:
Contraception during menopause
It is still possible to become pregnant if you have unprotected sex during perimenopause until you are certain that you have completely stopped having a menstrual cycle. This is usually 1 year after your last period if you’re over 50, and 2 years after for women under 50. Contraception is not needed after 55 years old.
Here is a useful guide for which contraception you can use during perimenopause and menopause:
Work related support
Menopausal symptoms can have a huge impact on your work life. A combination of disturbed sleep, hot flushes, brain fog and low mood can affect your attendance and performance, and research shows that some women reduce their hours or give up their jobs as a result.
Talk to your manager, get support, make changes and build a support network to help make a difference to your working life.
Kathy Abernethy – menopause, a workplace issue
Problems with menopause
If you are over 45 and experiencing menopause changes and symptoms, your doctor may wish to rule out any other conditions. If under 45 it is important to know for certain and blood tests may be required. If you are experiencing menopause symptoms that are affecting your daily life, you can talk to your doctor to discuss the different ways you can manage your symptoms in ways that are right for you.
Early menopause
When to get help with early menopause
Talk to your doctor about treatment options if you start the menopause early. Early menopause can affect both your physical and mental health and will affect your ability to have a baby. You’ll also have a higher chance of developing conditions such as osteoporosis and cardiovascular disease. The main treatment for early menopause is taking medicines such as the combined contraceptive pill or hormone replacement therapy (HRT) to replace your missing hormones.
If your menopause starts before you are 40, it is called premature ovarian insufficiency (POI).
Premature ovarian insufficiency (POI) explained – British Menopause Society
Menopause and cancer
Menopause and mental health
Some mental health symptoms, like occasional low moods, mild anxiety, brain fog and forgetfulness, are a normal part of the menopause, and can be very mild. Depression, regular anxiety, suicidal thoughts and psychosis are more serious, and you should talk to your doctor if mental health symptoms are having a negative impact on your life.
Symptoms can last for months or years and can change with time. Getting advice early can help reduce the impact perimenopause and menopause have on your mental health, relationships and work.
Menopause only affects you physically – truth or lie?
If you already live with a mental health problem, you may find the menopause affects it. Symptoms may get worse or become harder to manage, or medications may be less effective than before. Talk to your doctor if you are unsure.
Menopause and bipolar
For further information on mental health:
Menopause and other conditions
Menopause can have an impact on other conditions and may mean you need to change the way you treat your other conditions so that all your symptoms are managed effectively. If you have any concerns about existing conditions and the menopause, talk to your doctor.
Here are some common conditions that are affected by the menopause:
Cardiovascular disease
Coronary heart disease (CHD) explained
Chronic fatigue syndrome (CFS)
Some menopause symptoms are similar to symptoms of chronic fatigue syndrome (CFS), so is important to consult a doctor to determine the underlying cause and receive appropriate treatment
Menopause and endometriosis
Symptoms of endometriosis usually stop after the menopause – although it’s possible to have symptoms after menopause.
For further information on endometriosis, visit our page on gynaecology:
Irritable bowel syndrome (IBS)
If you already have IBS, your symptoms may become exacerbated by the hormonal changes during the perimenopause or menopause.
Osteoporosis
Osteoporosis explained
Pelvic organ prolapse
The decline in oestrogen levels during and after menopause can weaken the muscles and tissues in the pelvic area, including those that support the vagina, bladder and urethra. This can increase the risk of pelvic organ prolapse, and changes to bladder and bowel control.
For further information on pelvic organ prolapse, visit our page on pelvic health:
Local services
Specialist help
Specialist Doctor: Your doctor may refer you to a specialist doctor if you are experiencing particularly difficult symptoms that are not responding to standard treatment or your symptoms are particularly debilitating or complex, if you are unable to take HRT or your menopause has started early.
In Dorset, specialist services are provided by the Dorset Menopause Service run by University Hospitals Dorset.
Dr Abbie Laing from Dorset Menopause Service talks about Menopause
Specialist physiotherapy
Specialist Physiotherapy can help with some symptoms of the menopause such as losing control of bladder or bowel function or pelvic organ prolapse.
Specialist mental health
Your doctor may refer you to Dorset Mind’s Menopause Pathway as part of their Active Monitoring Programme.