Working better together
” We’ve all been working in our silos. We don’t know what the other [organisations] are involved in or what resources are available [in the] voluntary sector. There will be a number of projects that the council are running that we could work with, huge opportunities if we can just keep these talks going and keep people sitting around the tables.”
—
Joint Strategic Needs Assessment
Integrated care is about how we work better together. This means understanding how we need to work differently to implement the priorities and ambition in this strategy. Our vision is working together to deliver the best possible improvements in health and wellbeing. This section shares some insights about how we might achieve this when thinking about how our services need to change.
At a basic level, we should be moving more resources – such as money and people – to areas of health and care where needs are greatest. This could mean areas where health outcomes are not as good as the rest of the county, or health and care services that need more funding and people to provide high quality care.
For many years funding has flowed into our main health and care providers – the hospitals, our community and mental health trust and GPs. Most of the money is used to pay the salaries of the people needed to provide health and care. It can feel as if this has been organised in a way that suits how our health and care providers are used to working. We need to listen to people’s experiences and understand how to change this so that care is planned and delivered around people’s needs, not organisations.
How we collect and use information about you, and how we share it across our organisations, is also important to working better together. We’ve heard a lot from people who have not always experienced good communication when accessing health and care. We still ask people to repeat their story many times, and information about what matters to them is not always used to involve them in decisions about their care.
Alongside people and communities, our workforce will play a vital role in helping make these changes happen. We know there are shortages of key workers in parts of the health and care system, as well as more people needing to be seen, especially since services were reduced during the pandemic. When people don’t have a good health and care experience, it’s not because employees don’t care – pressures make it hard for them to provide care to the best of their ability.
We need to share our resources where they will make the most difference, and the starting point for this has to be understanding how best to meet people’s needs, not the needs of organisations. This is going to take time as it’s a new way of working, but together we’re confident that we can make a difference for people in Dorset.
Case study: prevention built in
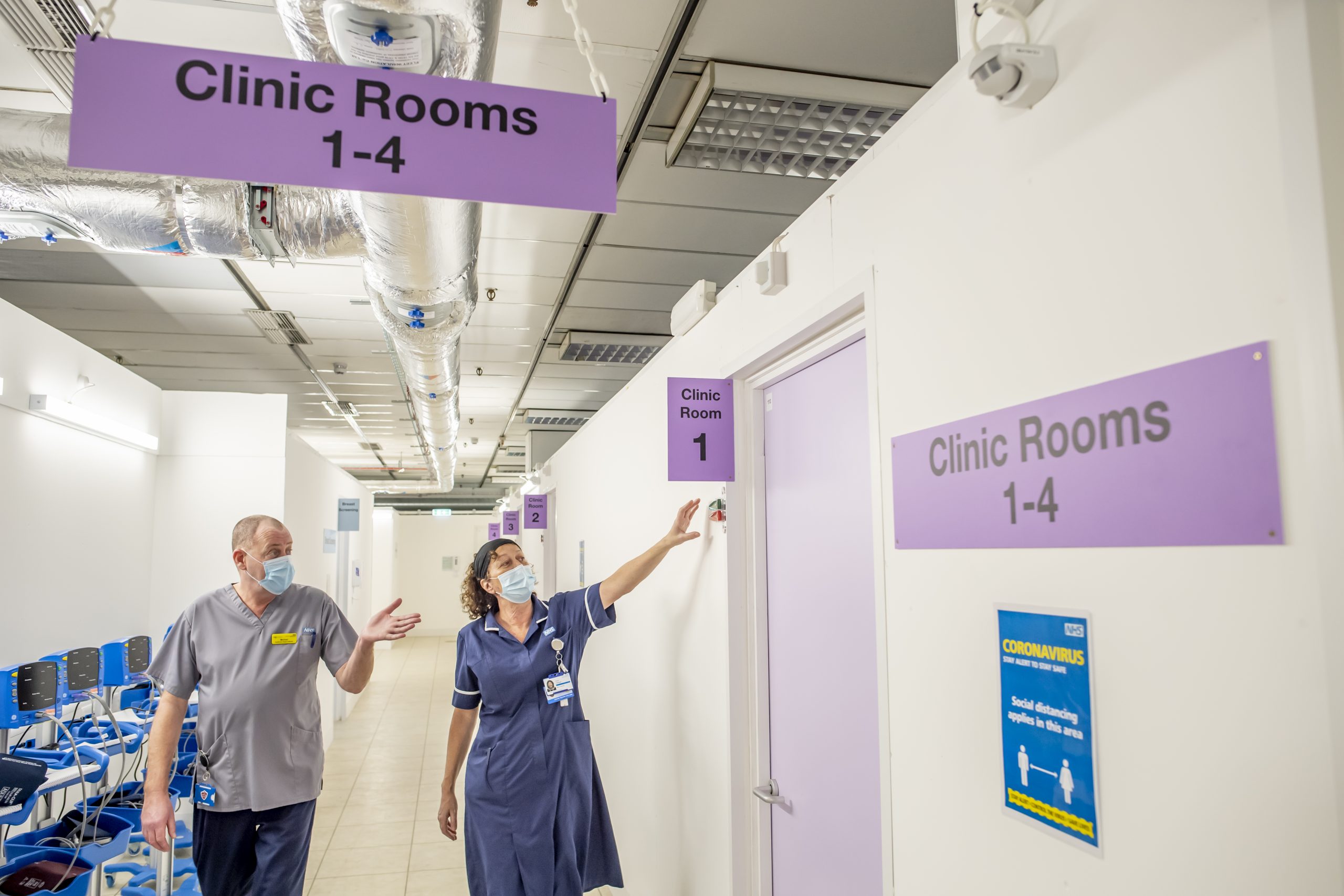
When waiting times grew for people needing surgery after the pandemic the local health service took a different approach. Extra clinics were needed to clear the waiting lists. These would review patients with joint problems who need orthopaedic surgery. Usually the solution would be to try to find extra space at our hospitals. But the Think Big project took the clinics to the high street in Dorchester and Poole instead. One clinic was at the former council headquarters close to the high street in Dorchester. The other was in the former Beales department store in the Dolphin Shopping Centre, Poole.
This was a chance to work in a different way. Traditional clinics would offer appointments to assess and prepare people for their surgery. At the new high street clinics, people receive advice on staying well, as well as information before their operation. Health coaches work alongside orthopaedic surgeons and physiotherapists to provide joined-up care.
The clinics have been open since April 2022. Since then health coaches have supported more than 2,790 people with advice to stay well. These were all people needing an orthopaedic operation who would not usually have such joined-up care. About six percent of these people have gone on to register for prevention help from the LiveWell Dorset service. But the most important part of this journey is the support and prompts to think about staying well.
As we develop integrated care, embedding prevention support at every opportunity will be a priority. Evidence shows that even very brief advice to be more active can lead one person in every 10 to take action. It doesn’t take much time, and is a fraction of the cost of treating the consequences of not being active enough.
Evidence shows that people have better health and wellbeing if they are cared for at or close to home compared with being in hospital.
Unfortunately, when admitted to hospital, older people can lose their independence and find it harder to return home. They may also develop further health issues because of changing their regular routine. Providing care closer to home is a key ambition for integrated care. It means you should receive more responsive, suitable care for you and your situation. It also means understanding what matters to you. If we are getting it right, you’ll will be able to make informed decisions and help design your own care.
This is not only good for you, it’s good for our planet too. Meeting your needs closer to home helps us reach our net zero targets for climate change. In 2018 people travelling to and from hospitals across Dorset generated an estimated 15,646 tonnes of CO2. This is the same as flying from the UK to Australia and back 2,688 times.
Our health and care system could also do more to improve health and wellbeing at an early stage. Prevention support can be effective, especially when people have a more serious health condition. When people need hospital care in Dorset, everyone is now offered support to quit smoking. And before many routine operations, people now receive lifestyle support from health coaches.
Care closer to home and prevention support at the same time as clinical care should be key ambitions for integrated care.
To get there we will need to understand how best to use data and information to help plan personal care. We also need to understand what is stopping us from working differently. Are there barriers for our workforce? How could information flow better between organisations? Can we collect information once from people, and understand their journey, making it as smooth as possible? How do we capture your needs and make this available to teams when needed? And what aspects of care and support are best carried out by the voluntary and community sector?
As people’s needs increase, technology can also help to keep people well without needing lots of care. We also want to offer help to people to regain independence after a crisis, without having to go to hospital first. Offering services early can often avoid the need for hospital or more intensive care.
In Dorset we have already developed some excellent data tools to identify people with higher risks, such as being frail, at risk of falling. We know from this data who is more at risk of having a poorer outcome. This data is important in understand how well we are implementing integrated care. But we must also ask people how well they feel supported and involved in their care. Together, this information will show whether we are making a difference.
Going forward:
1 year
3 to 5 years
5+ years
Going forward: